High-Risk Medications: Why They’re Different
You know what? When it comes to high risk medications patient safety, there’s no room for guesswork. Not all medications play by the same rules. Some are pretty forgiving—you miss a dose of ibuprofen or take it a little late, and maybe you just feel discomfort for a while. But then there are the heavy hitters—the high risk medications. These drugs operate on such a narrow margin that even the tiniest mistake can swing the outcome from healing to harm.
That’s why high risk medications patient safety isn’t just a medical buzzword—it’s a daily reality for providers and patients alike. These drugs are powerful, often life-saving, but they’re also unforgiving. A decimal in the wrong spot, a misread label, or even a harmless-looking herbal supplement can tip the balance.
Honestly, this is why healthcare professionals often look extra cautious when handling them. Ever seen a nurse pause, double-check, and then double-check again before administering a shot? That’s not paranoia—it’s a survival skill.
What Are High-Risk Medications in Nursing?
Let me explain. When someone asks, what are high risk medications in nursing? the answer boils down to this: they’re drugs where the cost of mistakes is unacceptably high.
Imagine insulin. It’s lifesaving, but too much? A patient can slip into hypoglycemia, complete with confusion, seizures, or even coma. Too little? Blood sugar spikes, putting stress on every organ in the body. Or consider anticoagulants like warfarin. Perfectly balanced, they prevent deadly clots. But a slightly wrong dose—or worse, mixing it with the wrong herb—can cause internal bleeding.
Here’s the thing: nurses know they can’t afford to treat these meds casually. That’s why many hospitals have systems requiring two nurses to check doses independently. And it’s also why more providers are learning about herb medication interactions—because supplements aren’t harmless add-ons, they’re part of the risk equation.
For a clear breakdown of high-risk drugs and their risks, you can always visit www.evaluatemymeds.com.
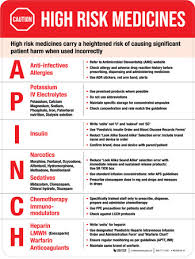
The List That Tells the Story
Every hospital maintains a list of high risk medications. And it’s not just paperwork or policy—it’s a hard-learned set of reminders, built from years of mistakes and lessons.
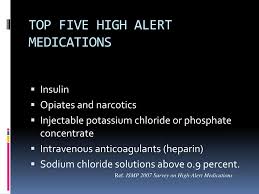
Some of the most common examples of high risk medications include:
-
Anticoagulants (Warfarin, Heparin): Great at preventing clots, but easy to overdose. Combine with the wrong herb? Risk skyrockets.
-
Insulin and Hypoglycemics: Precision drugs. Even a small error can send blood sugar crashing or soaring.
-
Chemotherapy Agents: Brutal but effective. They destroy cancer cells but can be toxic to healthy tissues and dangerous to handle.
-
Opioids and Sedatives: Vital for pain management, but misuse can suppress breathing. Too much, and patients literally stop breathing.
-
Potassium Chloride and Electrolytes: These keep your heart beating steadily. Get the dose wrong, and the rhythm falters—or stops.
What’s striking here isn’t just the danger. It’s the fact that these medications are used all the time. That’s why errors feel so gut-wrenching.
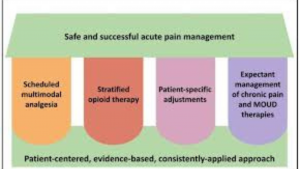
Managing High-Risk Drugs Without Panic

Here’s the thing: knowing the risks is only half the battle. The real challenge lies in managing high risk drugs in healthcare so that providers can use them confidently without constantly fearing disaster.
Doctors prescribe using standardized order sets, which cut down on miscommunication. Pharmacists double-check doses, run checks for interactions, and sometimes call providers back to clarify. Nurses scan barcodes before giving a drug—kind of like scanning groceries, but with life-or-death stakes.
Some hospitals even use color-coded storage bins or bold lettering to prevent look-alike drugs from being confused. Ever notice oversized, bold labels on IV bags? That’s not a design choice—it’s a safety tool.
Providers looking for structured strategies can find more guidance at www.evaluatemymeds.com.
The Quiet Risk of Herb–Drug Interactions

Now, let’s talk herbs. Patients love them, and many swear by them. But here’s the kicker: herb medication interactions can completely throw off treatment plans.
St. John’s Wort revs up the liver’s enzymes, making antidepressants or chemotherapy agents less effective. Ginkgo Biloba, taken for memory, can raise bleeding risks when mixed with warfarin. Garlic supplements can quietly tip a patient on anticoagulants into dangerous territory.
The real danger? Silence. Patients don’t always think of herbs as “real medications.” That’s how risky herb medication interactions sneak through.
That’s why a herb drug interaction checker is so valuable. It bridges the gap between the natural remedies aisle and the hospital pharmacy. Tools like the one at www.evaluatemymeds.com can catch interactions before they cause harm.
Patients Have Power Too

Medication errors aren’t just about what providers do. Patients can—and should—play an active role in medication safety for patients.
-
Keep a complete list. Prescriptions, OTC meds, and supplements. Write them down, carry them, and share them.
-
Ask questions. “What happens if I miss a dose?” “Can this interact with my morning tea?” Simple questions prevent big problems.
-
Use reminders. Pill boxes, sticky notes, or apps. Many even include built-in herb drug interaction checkers.
Patients who take these steps often feel more empowered. They stop being passive recipients and start being partners in care. For a step-by-step guide on patient safety strategies, check www.evaluatemymeds.com.
Technology to the Rescue
We live in a digital-first world, and technology is helping reduce medication errors. Electronic health records throw up alerts when risky combos are prescribed. Barcode scanning ensures the right drug goes to the right patient. Apps help people check interactions before they even leave the store.
Artificial intelligence is also stepping in, scanning massive datasets to predict which patients are most at risk for an error. It’s not replacing humans—it’s helping them stay sharp when fatigue sets in.
A Story That Could’ve Ended Better
A man recovering from heart surgery was prescribed warfarin. On his own, he started taking Ginkgo for memory. He never mentioned it because, well, “it’s just an herb.”
Weeks later, he was back in the hospital with severe bleeding. The culprit? A simple interaction that went unnoticed.
A quick run through a herb drug interaction checker could’ve prevented it. A single question—“Are you taking any supplements?”—could have saved him from the ordeal.
Wrapping Up: Safety Is a Shared Job
So what’s the bottom line? High risk medications patient safety isn’t the responsibility of one person or one role. Nurses need to understand what are high risk medications in nursing, doctors need to consult the list of high risk medications, and patients must embrace medication safety for patients.
Technology—barcode scans, EHR alerts, herb drug interaction checkers—is making it easier. But at the core, it’s the conversations, the pauses, the double-checks, and the shared responsibility that keep patients safe.
Honestly, safety may not be glamorous. It’s slow, repetitive, and sometimes feels tedious. But boring safety beats preventable harm every time.
Frequently Asked Questions (FAQ)

1. What are high risk medications in nursing?
High risk medications in nursing are drugs that have a higher chance of causing serious harm if used incorrectly. Examples include insulin, warfarin, opioids, and chemotherapy drugs. Nurses are trained to handle these medications with extra precautions—such as double-checking doses and monitoring patients closely—to protect high risk medications patient safety.
2. Can herbal supplements affect high risk medications?
Yes, they can. Herbal remedies like St. John’s Wort, Ginkgo Biloba, and garlic supplements may cause dangerous herb medication interactions. For example, Ginkgo combined with blood thinners like warfarin increases bleeding risk. This is why using a herb drug interaction checker before combining herbs with prescriptions is so important.
3. What are some examples of high risk medications?
Some of the most common examples of high risk medications include anticoagulants (like heparin), insulin, opioids, sedatives, chemotherapy agents, and concentrated electrolytes like potassium chloride. These are often listed on a hospital’s official list of high risk medications to remind providers of the risks.
4. How can patients improve medication safety?
Patients can improve medication safety for patients by keeping an up-to-date list of all prescriptions, over-the-counter drugs, and supplements. They should also ask their providers about possible interactions, use reminders or apps to avoid missed doses, and mention herbal products during appointments. Simple steps can dramatically improve high risk medications patient safety.
5. How are high risk drugs managed in healthcare settings?
Hospitals approach managing high risk drugs in healthcare through layered safeguards: standardized prescribing templates, pharmacist reviews, barcode scanning, and nurse double-checks. Many systems also integrate herb drug interaction checkers to flag hidden risks before they cause harm. These measures reduce errors and build stronger patient trust.
External Link:
-
Institute for Safe Medication Practices (ISMP) – High Alert Medications
-
Centers for Disease Control and Prevention – Medication Safety Program
Internal Link:
-
herb drug interaction checker: https://evaluatemymeds.com/
-
medication safety for patients: https://evaluatemymeds.com/index.php/blog/