Why This Conversation Matters

Honestly, when was the last time you sat down and thought about the pills in your medicine cabinet? Probably never, right? Most of us take our meds, wash them down with coffee or water, and move on with our day. But here’s the thing—some medications aren’t so forgiving. They fall into a special category: the top high risk medications. And these aren’t the ones you want to be casual about.
We’re talking about insulin, blood thinners, opioids, chemo drugs, and sedatives. Lifesaving? Absolutely. But they can also flip on you with the smallest mistake—too much, too little, or mixed with the wrong thing. And you know what’s sneaky? It’s not just the meds themselves. Herbs, teas, and supplements—those “all natural” things you pick up at a health shop—can quietly stir up herb medication interactions that nobody warned you about.
Now, hospitals have guardrails. Nurses rely on protocols like a nursing high risk medications guide. Machines scan barcodes. Pharmacists double-check orders. At home, though? It’s just you, your meds, and maybe a few vitamins sitting in that cluttered drawer next to the band-aids. That’s why learning how to manage high risk drugs safely matters—it’s not extra credit; it’s basic survival.
So this isn’t just a list. Think of it as a conversation—a mix of categories, real stories, everyday comparisons, and gentle reminders. Because medication safety isn’t abstract; it’s personal.
What Makes a Medication “High-Risk”?

Let me explain it this way: some medications are like driving a car on a quiet country road. Even if you drift a little, you’re probably fine. Others? They’re like threading a semi-truck through a narrow mountain pass in a snowstorm. One wrong move, and you’re in trouble. That’s the difference.
These high-risk medications have what doctors call a narrow therapeutic window. That’s just a fancy way of saying the safe zone between too little and too much is razor-thin. Patients don’t care about the jargon. They care about the reality—one skipped dose could cause a clot; one extra pill could put you in the ICU.
Take warfarin, a classic blood thinner. Forget a dose? You’re risking clots. Take a little extra? A bruise from bumping your arm on a counter could balloon out like something from a horror movie. Or insulin—miss it, and your blood sugar creeps higher than a holiday pie binge. Take too much, and you’re shaky, sweaty, maybe unconscious before your sandwich is done toasting.
And food? Yes, even food gets involved. Spinach, kale, collard greens—they’re healthy. But for someone on warfarin, that vitamin K can mess with how the drug works. It’s not about banning salads. It’s about consistency. Think of it like baking—change the recipe slightly, and suddenly your cookies don’t rise.
The Big Five Categories That Raise Red Flags

Instead of rattling off endless drug names (who remembers those anyway?), let’s group them. These five categories are the usual suspects:
-
Blood thinners (anticoagulants)
-
Insulin and other hypoglycemics
-
Opioids and strong painkillers
-
Chemotherapy drugs
-
Sedatives and benzodiazepines
Blood Thinners: Lifesavers with Sharp Edges

Anticoagulants keep your blood from clotting dangerously. They’re heroes for people at risk of strokes or heart attacks. But they’re also infamous on every list of high risk medications in healthcare. Too much, and bleeding becomes uncontrollable. Too little, and clots sneak through.
Here’s where it gets tricky: herbs. Garlic in your stir-fry, ginkgo in your tea, ginger in your smoothie—they can thin blood too. Stack them with warfarin, and suddenly you’re bleeding from the tiniest cut. That’s a textbook herb medication interaction.
You know what’s easy, though? Running those combos through an herb drug interaction checker. It’s like checking the weather before leaving the house—you may not need an umbrella, but you’ll be glad you looked.
Insulin: The Balancing Act

Living with diabetes is like juggling oranges. Add insulin, and suddenly you’re juggling flaming torches. The margin for error is thin. Too little insulin, and blood sugar climbs. Too much, and you’re dizzy, maybe unconscious.
It’s no wonder insulin tops the examples of high risk medications. In hospitals, nurses take it seriously—sometimes requiring two people to check a single dose, following the nursing high risk medications guide. At home, though, people are juggling insulin with mealtimes, stress, and sometimes herbal remedies like cinnamon or bitter melon.
And here’s the surprise: those herbs lower blood sugar too. Combine them with insulin, and your levels might plummet like a roller coaster. Again, an herb drug interaction checker is your friend here.
Opioids: Relief That Comes with Strings

Opioids are powerful pain relievers—sometimes the only thing that works. But they’re also magnets for misuse. Addiction, overdose, respiratory depression—they’re why opioids always make the list of high risk medications in healthcare.
And here’s the thing: the real risk often comes from combinations. A couple of glasses of wine, a sleep aid, maybe valerian root tea—it all piles up. What felt safe can suddenly be dangerous. In hospitals, staff stick to protocols outlined in the nursing high risk medications guide. At home? It’s easy to misjudge.
Chemotherapy: Precision Required

Chemo drugs are like laser beams—they need pinpoint accuracy. Too strong, and they damage healthy cells. Too weak, and cancer cells slip by. That’s why hospitals enforce the strictest high alert medications patient safety protocols for chemo.
But patients often want to support their bodies with supplements. Turmeric, green tea extract, echinacea—they sound harmless. But they can change how chemo drugs are absorbed. Without an herb drug interaction checker, you might never know your supplements are working against your treatment.
Sedatives: Small Pills, Big Consequences

Sedatives—diazepam, lorazepam—help with anxiety, seizures, and sleep. But they slow reflexes, impair memory, and increase fall risk, especially in older adults. They’re also addictive.
Mix them with alcohol or herbs like kava, and sedation doubles up. That’s why they’re considered prime examples of high risk medications. They may look small, but their impact is outsized.
Herbs: The Natural Trouble-Makers

Let’s pause. Why do so many people trust herbs more than prescriptions? Maybe it’s the word “natural.” Maybe it’s cultural tradition. But “natural” doesn’t mean “harmless.” Herbs interact with your liver enzymes, the same way prescriptions do.
Some troublemakers worth repeating:
-
St. John’s Wort + Antidepressants → Too much serotonin, even dangerous.
-
Ginkgo + Warfarin → Bleeding risk skyrockets.
-
Garlic + Insulin → Unpredictably low blood sugar.
That’s why using an herb drug interaction checker is smart. Think of it like Yelp for supplements—better to know the reviews before you try the dish.
Building a Home Safety System

Hospitals have barcodes and scanners. At home, you’ve got habits. Good ones make all the difference. Here’s what how to manage high risk drugs safely looks like:
-
Read the label. Every time. Even if you think you know it.
-
Get organized. Pill organizers, alarms, apps—whatever keeps you on track.
-
Check before mixing. Don’t assume supplements are harmless.
-
Tell your doctor everything. Even your bedtime tea.
-
Write it down. A simple note can stop a double dose.
It’s not complicated, but it is important. Honestly, these small steps are the fence at the top of the cliff—not the ambulance at the bottom.
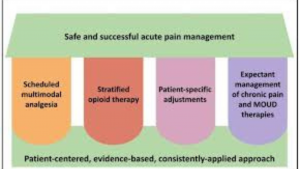
Nurses: The Safety Guardians

Nurses are the unsung heroes of medication safety. They don’t rely on memory alone. They’ve got the nursing high risk medications guide, which spells out protocols: double-check doses, avoid shorthand, document everything.
Sometimes it takes two nurses to give one dose of insulin. Sounds over the top, but you know what? It works. At home, you can mimic the same idea—slow down, double-check, ask someone else to confirm.
Hospitals: Layers of Safety Nets

Hospitals build redundancy into everything. Barcode scanning ensures the right pill goes to the right patient. Electronic prescribing prevents mistakes from messy handwriting. Checklists enforce accountability. All of this falls under high alert medications patient safety.
But don’t underestimate your role. Patients who ask questions—“What’s this for?” or “Is that my usual dose?”—often catch errors. Safety is a partnership, not a one-way street.
Real Stories That Hit Home
Stories stick longer than statistics. Here are a few that illustrate why this matters:
-
A man on warfarin added ginkgo to improve memory. Days later, he was rushed to the hospital with internal bleeding.
-
A woman with diabetes accidentally doubled her insulin dose one morning. By lunch, she was unconscious.
-
A cancer patient started turmeric supplements during chemo. Her treatment became less effective.
These aren’t “what ifs.” They’re lived experiences—sobering examples of high risk medications gone wrong.
A Checklist You’ll Actually Use

Here’s a quick, practical checklist:
-
Know your list of high risk medications in healthcare.
-
Keep your meds organized and consistent.
-
Run every herb or supplement through an herb drug interaction checker.
-
Borrow from the nursing high risk medications guide—check, confirm, record.
-
Remember: high alert medications patient safety is a team effort.
Wrapping It Up
The top high risk medications aren’t villains. They’re powerful, necessary tools. But they need respect.
By staying alert to herb medication interactions, using an herb drug interaction checker, and learning how to manage high risk drugs safely, you protect yourself and your loved ones.
So slow down. Ask the extra question. Read the label again. Check that supplement before you take it. Because sometimes, that one small pause is what makes the difference between safety and danger.
Frequently Asked Questions (FAQ)
1. What are considered the top high risk medications?
The top high risk medications typically include insulin, anticoagulants (blood thinners), opioids, chemotherapy drugs, and sedatives. These medications have a higher chance of causing serious harm if they’re taken incorrectly.
2. Why are these medications called “high risk”?
They’re called high risk because the difference between a safe dose and a harmful one is very small. Even slight errors in timing, dosage, or mixing them with herbs or supplements can lead to severe side effects or complications.
3. How can I manage high risk drugs safely at home?
To practice how to manage high risk drugs safely, use a pill organizer, set reminders, read labels carefully, and keep a medication log. Always check for interactions with herbs and supplements using an herb drug interaction checker, such as the one at www.evaluatemymeds.com.
4. Do herbs and supplements really interact with medications?
Yes. Many herbs can cause dangerous herb medication interactions. For example, ginkgo and garlic can increase bleeding risk when taken with blood thinners, and cinnamon or bitter melon can drop blood sugar too low when combined with insulin.
5. What role do nurses play in medication safety?
Nurses follow structured protocols, often outlined in a nursing high risk medications guide, to reduce errors. They double-check doses, monitor patients closely, and document every step. These safety habits can also be adapted at home.
6. Where can I find a reliable list of high risk medications in healthcare?
The Institute for Safe Medication Practices (ISMP) and the FDA provide updated lists of high risk medications in healthcare. You can also explore detailed resources and guides on www.evaluatemymeds.com.
🔗 External Link:
-
Institute for Safe Medication Practices (ISMP) List of High-Alert Medications
-
National Center for Complementary and Integrative Health (NCCIH): Herbs and Supplements
🔗 Internal Link:
-
Check your medications for risks → https://evaluatemymeds.com/
-
Understanding herb-drug interactions → https://evaluatemymeds.com/index.php/blog/
-
Medical Terms Made Easy → https://evaluatemymeds.com/index.php/glossary-simple-medical-terms/
-
Understanding your medical reports → https://evaluatemymeds.com/index.php/understand-my-medical-document/