Introduction: That Moment When the Medication List Starts Looking… A Little Wild
![]()
You know what? Nearly every pain patient reaches a moment where they hold their prescription list in their hand, stare at the names, and think, “Why am I taking all of these together?”
Especially when the list includes opioids, gabapentin, NSAIDs, and a PPI. It looks like a full-on pharmacy lineup, not something one person should need just to get through the day. Honestly, you’re not wrong for wondering. Most people don’t get much of an explanation; they just get a stack of prescriptions and maybe a “take with food” sticker.
But here’s the thing: pain doesn’t arrive in a neat, single package. It can burn, throb, pulse, ache, tighten, and flare up—sometimes in the same afternoon. And because pain behaves like a wild mix of electrical and inflammatory chaos, doctors often treat it with layered medications rather than throwing one pill at the problem and hoping for the best.
This is why the combination approach exists. And once you understand what each medication actually does—and how they support one another—it starts making much more sense.
We’re going to break it all down in a real, human way. No stiff textbook voice. Just clarity
Pain Isn’t Just “Pain” — It’s an Entire Cast of Characters

Pain Behaves More Like a Weather System Than a Simple Symptom
If you’ve lived with chronic pain, you already know it changes from day to day. Some days, it’s a dull heaviness. Other days, it’s a lightning strike down your leg. And occasionally, it’s both.
Honestly, I sometimes think pain is like a stubborn storm sitting over the Midwest—one day it dumps rain, the next it hits you with a cold snap. And because pain has so many “faces,” treating it often requires more than one tool.
That’s why doctors use combinations. They’re not trying to overwhelm you—they’re trying to match treatment to the way your pain actually behaves.
Different medications target different aspects:
-
Nerve pain: that buzzing, burning, shocking sensation
-
Inflammatory pain: deep swelling, stiffness, heat
-
Breakthrough pain: those sudden spikes that hijack your day
-
Side-effect protection: especially for your stomach
Let me explain something that surprises a lot of people: one pain type can irritate another. When inflammation is high, nerves get touchier. When nerve pain is severe, muscles tense and swell. It becomes a whole cycle.
That’s why your treatment looks layered—it is layered.
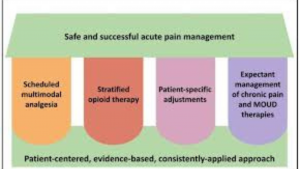
Why Doctors Often Pair Opioids and Gabapentin
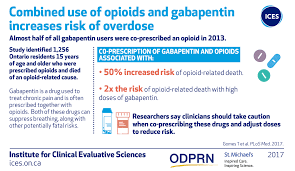
The Opioid + Gabapentin Combo: Not a Mistake, Not a Duplicate
A common question is:
“Why would a doctor prescribe opioids and gabapentin together?”
And you know what? It’s a completely valid question, because at first glance it looks like doubling up. But these two medications work in totally different ways.
Opioids block pain signals higher up—closer to the brain.
Gabapentin calms irritated nerves further down the chain.
It’s like trying to quiet a neighborhood with noise coming from two different houses. The opioid handles one house, gabapentin handles the other. And when both quiet down, the neighborhood (a.k.a. your nervous system) finally gets a break.
Why this combination helps so many people
-
It reduces nerve hyperactivity
-
It prevents pain spikes from becoming overwhelming
-
It helps lower the opioid dose
-
It builds a steadier baseline of relief
But—here’s the thing—because these medications both influence the nervous system, doctors monitor them closely. Not because they’re “dangerous,” but because the combination needs balance.
A small tangent here: herbs matter too. A lot. Herbs like valerian, kava, or CBD can magnify calming effects, sometimes more than people expect. That’s why checking combinations with a herb interaction tool (there are several online) is smart, not paranoid.
Just a quick note I’ll repeat again later: herbs absolutely can interact with pain meds. And people often find that out only after feeling extra drowsy or “off” without knowing why.
Why NSAIDs Often Come With PPIs

The Anti-Inflammatory + Stomach Protection Duo
NSAIDs are fantastic for inflammation. No question. They reduce swelling, stiffness, and that deep joint ache that feels like it sits in your bones. But they’re also known to irritate the stomach lining—especially when you take them for more than a few days.
So what do doctors do?
They add a PPI to protect your stomach.
It’s not overkill. It’s prevention.
Think of it like eating spicy food. Sure, you can enjoy the heat—but many people keep a glass of milk or a soothing drink nearby to keep things under control. PPIs are that soothing drink.
This is especially important if you:
-
Take NSAIDs daily
-
Have reflux
-
Use blood thinners
-
Are over 50
-
Have a history of stomach sensitivity
Another quick aside: People often take turmeric or ginger for inflammation, assuming they’re harmless. But both can amplify bleeding risk when paired with NSAIDs. Just something to tuck away in your mind.
How All Four Medications Work Together

A Layered Strategy Makes More Sense Than One Medication Ever Could
Here’s the thing: no single medication can handle the variety of pain signals firing inside a chronic pain patient’s body. Not realistically.
Pain management is much more like cooking a full meal. You don’t make chili with just beans. You need seasoning, broth, vegetables, maybe beef or turkey—each ingredient brings something different to the dish. And if one is missing, the whole balance is off.
Your medication plan works in the same way:
-
Gabapentin → nerve pain
-
NSAIDs → inflammation
-
Opioids → sudden spikes
-
PPIs → stomach protection
When all four are used intentionally, the day becomes a little more manageable.
A slight tangent: some patients tell me they can actually feel which medication is helping which type of pain. Others can’t. Both experiences are completely normal. Everybody’s body speaks a different “pain language.”
When This Plan Works Well — And When It Doesn’t
The combination works beautifully when:
-
Pain is coming from nerves + tissue + unpredictable flares
-
You need long-term stability
-
NSAIDs irritate your stomach
-
You’re trying to keep opioid doses lower
But it becomes tricky when:
-
People accidentally take two NSAIDs (like ibuprofen + naproxen)
-
Alcohol is thrown into the mix
-
Herbs amplify sedative effects
-
Kidney or liver concerns appear
-
Meds aren’t taken with food
-
Supplements are added without guidance
You know what often causes the biggest surprise? A “natural” product interacting with a prescription.
It happens way more often than people expect.
Herbs, Supplements, and the Curveballs They Can Throw

Natural Doesn’t Always Mean Neutral
We live in a time when herbal blends, wellness teas, CBD gummies, and mushroom powders are everywhere—Instagram, grocery stores, even gas stations. And while many are genuinely helpful, they’re not always harmless when mixed with prescription medications.
For example:
-
CBD slows the breakdown of several medications
-
Kava amplifies sedation
-
Turmeric increases bleeding risk
-
Kratom interacts with opioid receptors
-
Ginger and garlic supplements affect platelets
-
St. John’s Wort lowers medication levels
Some of these interactions can be mild. Others can shift how medications work entirely.
It’s kind of like mixing cleaning products—you don’t always realize that two harmless bottles can create fumes when combined.
So checking interactions is not “being too careful.” It’s just smart.
Using a Herb Interaction Checker Makes Life Easier
Most good interaction checkers allow you to enter:
-
Your prescriptions
-
Your herbs
-
Your vitamins
-
Your supplements
-
Your over-the-counter meds
Then they show you whether the combination is safe, needs a dosage adjustment, or should be avoided.
Let me explain why this matters: it prevents you from accidentally combining something like gabapentin with a strong sleep herb and wondering why you feel dizzy or foggy. It saves you a lot of guessing—and a lot of unnecessary discomfort.
What a Safe Long-Term Pain Plan Actually Looks Like

A Steady Plan Is More About Balance Than Complexity
A safe long-term plan usually includes:
-
Consistent timing
-
No duplicate medications
-
Regular check-ins with your provider
-
Honest discussion about herbs and OTC items
-
Lab work when needed
-
Tracking how your body responds
-
A reliable interaction checker
It’s not about having the fewest medications. It’s about having the right ones working together.
Many patients using opioids, gabapentin, NSAIDs, and PPIs eventually settle into a rhythm. It doesn’t mean the pain is gone—but life becomes a bit more predictable.
And predictability is a small win that matters a lot more than people think.
Conclusion: Pain Relief Should Feel Understandable, Not Overwhelming
If your medication list includes opioids, gabapentin, NSAIDs, and a PPI, there’s a reason. A thoughtful one. These medications aren’t thrown together randomly—they’re chosen to support different parts of your pain experience and to protect your body while doing so.
Now you know why the combination exists, how each medication plays its part, how herbs can shift things, and how a simple interaction check can prevent a lot of frustration.
Pain may be messy. But your treatment plan shouldn’t feel mysterious.
You deserve clarity, you deserve relief, and you deserve to feel confident in the care you’re receiving.
External Link
Medication Mechanisms & Safety
-
CDC Opioid Basics
https://www.cdc.gov/opioids/basics -
NIH Gabapentin Fact Sheet
https://www.ncbi.nlm.nih.gov/books/NBK493228/ -
Mayo Clinic NSAID Safety Guidance
https://www.mayoclinic.org/drugs-supplements-nsaids -
Cleveland Clinic PPI Overview
https://my.clevelandclinic.org/health/treatments/21878-proton-pump-inhibitors-ppis
Herb–Drug Interactions
-
MedlinePlus: Herb & Supplement Interactions
https://medlineplus.gov/druginformation.html -
Memorial Sloan Kettering Herb Database
https://www.mskcc.org/cancer-care/diagnosis-treatment/symptom-management/integrative-medicine/herbs -
NIH Office of Dietary Supplements
https://ods.od.nih.gov
Pain Management Guidelines
-
American Chronic Pain Association
https://www.theacpa.org -
FDA Medication Guide Library
https://www.fda.gov/drugs/drug-safety-and-availability/medication-guides
Internal Link
FAQ Section
Frequently Asked Questions
1. Why am I prescribed opioids, gabapentin, NSAIDs, and a PPI all at once?
These medications target different pain pathways. Your doctor may be combining them to reduce nerve pain, inflammation, and sudden flare-ups while also protecting your stomach. You can upload your full medication list to www.evaluatemymedscom to understand the purpose behind each one.
2. Is it safe to take these medications together long-term?
It can be safe when monitored, but combinations must be reviewed regularly. If you’re unsure, www.evaluatemymedscom can help verify whether your regimen is still appropriate.
3. Can herbs or supplements interfere with my pain medications?
Absolutely. Herbs like turmeric, CBD, kava, or St. John’s Wort may cause unexpected interactions. Check your full list using the herb interaction tool on www.evaluatemymedscom.
4. What symptoms should I watch for when taking these medications together?
Watch for dizziness, stomach pain, sedation, swelling, trouble breathing, or confusion. If anything feels “off,” upload your symptoms and medications to www.evaluatemymedscom to get a clearer picture.
5. Where can I get a full, simplified explanation of my medication plan?
If your medication list feels overwhelming, www.evaluatemymedscom can provide a simple, clear breakdown — including food interactions, herb safety, and medication combinations.