Introduction: Why Recognizing High Risk Medications in Healthcare Matters
Recognizing high risk medications in healthcare isn’t just a checklist—it’s a life-or-death skill. Imagine a nurse on a hectic night shift mixing up insulin types, or a patient quietly taking St. John’s Wort alongside blood thinners. These aren’t rare scenarios. They happen every day, and the consequences can be devastating.
That’s why healthcare professionals and patients alike need to understand what are high risk medications in nursing, why hospitals rely on the common high risk medications list, and how real-world errors become examples of high risk medications in hospitals.
At www.evaluatemymeds.com, we emphasize not just the professional side of safety but also the patient’s role in awareness. From safely managing high risk medications to preventing silent herb medication interactions, recognition and vigilance protect lives.
What Are High Risk Medications in Nursing and Healthcare?

So, what are high risk medications in nursing and the wider healthcare world? These are the drugs that don’t forgive mistakes. Insulin, anticoagulants, opioids, chemotherapy agents—powerful medicines with razor-thin margins.
They’re everywhere: ICUs, emergency rooms, nursing homes. That’s why recognizing high risk medications in healthcare isn’t memorization—it’s habit. Pausing to verify, questioning doses, double-checking vials—these small actions are what stand between safety and harm.
Why Recognition Equals Safety

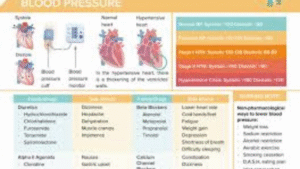
So why all this fuss? Because patient safety is fragile. Systems exist to catch errors—automated dispensing machines, barcode scanners, electronic prescriptions—but no system is perfect. A smudged label, a rushed click, a tired eye, and suddenly, safeguards crumble.
That’s where high alert medications patient safety measures step in. Think brightly colored stickers shouting, “Check me twice.” Think storage cabinets that physically separate risky drugs. Tall-man lettering (HYDROmorphone vs. morphine) that forces your brain to slow down.
And yet, here’s the catch: these are just aids. They don’t replace awareness. Safely managing high risk medications depends on professionals who stay skeptical, even suspicious. They ask: “Is this dose right? Is this the right patient? Am I missing something?” That edge of doubt isn’t weakness—it’s wisdom.
The Medications Everyone Watches Closely

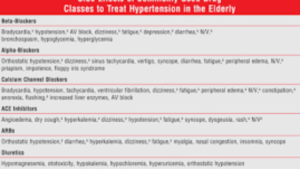
Here’s a quick walk-through of the common high risk medications list—the drugs every healthcare worker treats with extra care:
-
Anticoagulants (Warfarin, Heparin, DOACs): Lifesavers against clots, but bleeding is the constant shadow.
-
Insulin: A daily reality for millions, but decimals matter. A “.5” vs. “5” mistake? Disaster.
-
Opioids (Morphine, Fentanyl, Hydromorphone): Heroes for pain relief, but unforgiving when overdosed.
-
Chemotherapy agents: Toxic by design—exact dosing is the only safe way.
-
IV Potassium: Essential for the heart, but deadly if infused too fast.
This common high risk medications list evolves, and keeping up is part of the job. Think of it like updating software—you can’t run old knowledge on new systems.
At www.evaluatemymeds.com, we’ve seen how reviewing this common high risk medications list with patients builds understanding and strengthens trust.
Hospital Stories That Hit Hard

Let’s get honest. Reading about risk lists doesn’t punch you in the gut like hearing actual stories. Here are examples of high risk medications in hospitals that stick:
-
A patient recovering from surgery gets the wrong insulin type. Within 30 minutes, their blood sugar nosedives, and a code blue blares overhead.
-
A decimal point error in chemotherapy multiplies a dose tenfold. The patient survives, but with long-term organ damage.
-
Hydralazine (blood pressure) mistaken for hydroxyzine (allergy). The patient’s blood pressure plummets, and a stable case turns critical.
You know what’s striking? These aren’t freak accidents. They’re the result of everyday pressures—fatigue, rushing, distractions—that make professionals human. That’s why recognizing high risk medications in healthcare can’t be passive. It’s active, constant, and relentless.
Managing Risk in the Real World
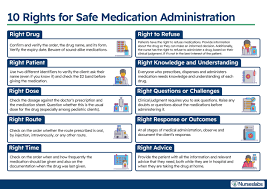
So how do professionals cope with this reality? Safely managing high risk medications is part skill, part habit, and part culture.
-
Double-checks: Two people, independently, reviewing the order. Some call it redundant. But when the risk is life or death, redundancy is resilience.
-
Technology: Barcoding and smart infusion pumps are like safety nets. Not perfect, but they catch slips.
-
Clear communication: No shorthand, no ambiguous abbreviations. Writing “.5” instead of “0.5” has caused too many tragedies.
-
Continuous training: Knowledge isn’t static. Teams review the common high risk medications list, refresh protocols, and share lessons from near misses.
-
Patient engagement: Teaching patients their meds isn’t just courtesy—it’s defense. A patient who knows their insulin should be “long-acting” might catch an error before harm happens.
And here’s a thought: safety isn’t about perfection. It’s about layers. Each safeguard catches what the last missed. Together, they build a net strong enough to hold.
At www.evaluatemymeds.com, we encourage providers to use these layers together—they weave a net strong enough to catch errors before harm happens.
The Supplement Problem Nobody Talks About Enough

Now, let’s shift to the sneaky part: herb medication interactions. Supplements are booming—walk into any drugstore or scroll TikTok wellness trends, and you’ll see people pushing turmeric shots, ginseng teas, and ashwagandha capsules. They look harmless. But they’re not always.
-
St. John’s Wort speeds up liver enzymes. Translation? It can flush out life-saving drugs too fast—blood thinners, antidepressants, even cancer meds.
-
Ginkgo Biloba makes platelets less sticky. Great for memory, maybe. But when paired with aspirin or warfarin? Suddenly, bleeding risks skyrocket.
-
Turmeric has anti-inflammatory properties, but in high doses, it can interfere with certain chemotherapy drugs.
The real issue? Patients often don’t mention supplements. Maybe they think, “It’s just tea.” Or maybe they fear judgment. That silence makes herb medication interactions one of the most under-discussed dangers in healthcare.
Tools That Actually Help
So how do we bridge that gap? Enter the herb drug interaction checker. It’s exactly what it sounds like—a digital tool that flags dangerous combos between herbs and prescription meds.
Picture a pharmacist reviewing a patient’s list: warfarin for clot prevention, ginseng for energy. Plugging those into a checker like Drugs.com, Medscape, or Lexicomp instantly shows the bleeding risk. Crisis averted, before it even starts.
And you know what? These tools aren’t just for pros. Patients can use them too. Imagine being able to check your chamomile tea against your antidepressant from your phone. It puts some control back in patients’ hands, and that’s huge.
Adding a herb drug interaction checker into the workflow doesn’t just support safely managing high risk medications. It expands the definition of safety to include the hidden world of supplements that’s often overlooked.
At www.evaluatemymeds.com, we encourage providers to use these layers together—they weave a net strong enough to catch errors before harm happens.
Nurses: The Unsung Heroes

Let’s pause for a moment to acknowledge something. What are high risk medications in nursing practice? They’re the daily reality of frontline care. Nurses don’t just administer these meds. They prepare them, double-check them, explain them to patients, and watch the effects unfold in real time.
It’s heavy. Imagine being the last person between a vial and a patient’s bloodstream. Imagine noticing a decimal that doesn’t look right, or a label that seems smudged, and realizing your catch just prevented a catastrophe. That’s what nurses do every day.
That’s also why recognizing high risk medications in healthcare so often relies on nursing vigilance. They are the eyes, ears, and voices that bring high alert medications patient safety systems to life.
Safety Protocols That Matter

Sometimes protocols feel like red tape. But when it comes to high alert medications patient safety, they’re lifelines:
-
Tall-man lettering: HYDROmorphone vs. morphine. That capitalization trick reduces look-alike errors.
-
Separate storage: Keeping high-risk meds apart, with bold labels and warnings.
-
Restricted access: Limiting administration of chemotherapy, for example, to trained staff.
-
Mandatory verification: Two professionals, two signatures, one patient safe.
These aren’t bureaucratic hoops. They’re seatbelts. They don’t stop the crash, but they keep you alive when it happens.
Habits That Make the Difference

For professionals, the small habits matter most:
-
Keep the common high risk medications list nearby—on a pocket card, phone app, or pinned on the wall.
-
Always run supplements through a herb drug interaction checker—don’t leave it to chance.
-
Take double-checks seriously, even when the ward feels like chaos.
-
Teach patients the names and purposes of their meds. An informed patient is an extra layer of safety.
-
Share stories. Near misses, close calls—they’re lessons, not embarrassments.
This is how a culture of safety builds: small, repeated actions that stack into resilience.
At www.evaluatemymeds.com, we encourage professionals and patients alike to build these habits into their routines.
FAQ: Recognizing High Risk Medications in Healthcare Made Simple
1. What are examples of high risk medications in hospitals?
Insulin, anticoagulants, opioids, chemotherapy agents, and IV potassium.
2. What are high risk medications in nursing practice?
Drugs nurses must handle with extreme care, including insulin, opioids, and anticoagulants.
3. Why do herbs matter with prescriptions?
Because herb medication interactions can alter how drugs work, making them too strong or too weak.
4. How does a herb drug interaction checker help?
It instantly shows risks between herbs and prescriptions—vital for both professionals and patients.
5. What’s the safest way to manage high risk drugs?
By combining safely managing high risk medications protocols, patient involvement, and strong high alert medications patient safety systems.
External Links:
Internal Links:
-
Blog on Polypharmacy Risks – https://evaluatemymeds.com/index.php/blog/
-
Herb-Drug Interactions Page – https://evaluatemymeds.com/
-
Understanding your medical reports – https://evaluatemymeds.com/index.php/understand-my-medical-document/
-
Medical Terms Made Easy – https://evaluatemymeds.com/index.php/glossary-simple-medical-terms/